Femtosecond Laser in Cataract Surgery: What Makes it Worth it? or not?
Abstract
This review is designed to look at a prospective evaluation of the use of the femtosecond laser and manual incision standard cataract surgery in one center with one surgeon focusing on visual outcomes and complications. Multiple studies support both benefits, risks, alternatives, and differences between manual capsulotomy combined with standard manual incision cataract surgery and cataract surgery employing the femtosecond laser in conjunction with routine phacoemulsification. The purpose of this study was to evaluate early postoperative outcomes using a prospective evaluation of cases from one surgeon over the course of two years from 2015-2017. The first group of cases involves 2134 eyes comparing phacoemulsification time in seconds (PT), ultrasound time in seconds (UT), and cumulative delivered energy (CDE). The second group of cases involves 1913 eyes that were Lens Opacification Classification III similar and without other ocular or lenticular abnormalities. Finally, a subgroup from the latter group (n=150) were evaluated over the course of two days and postoperative 3-hour examinations (visual acuity) were compared.
Author Contributions
Academic Editor: Min Zhao, Post-doctoral Research Associate, China
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2018 Karl Stonecipher, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Cataract surgery and techniques are constantly evolving. These changes range from completely new surgical concepts (pathbreaking innovations), modification of a single procedural step and customization of techniques to fit personal surgical talents. The use of femtosecond lasers in cataract surgery was introduced by Nagy et al. in 2009. 1 Other surgeons followed with publications documenting the theoretical, scientific and practical benefits of the femtosecond laser. 2, 3 Soon after its introduction, surgeons began to discuss the pros and cons of the use of the femtosecond laser in cataract surgery. 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14 Several major reviews, both positive and negative, have been published. It is the intent of this study to present the immediate visual benefits and safety roughly ten years after the introduction of this technology in cataract surgery. 15, 16, 17, 18, 19 It is not the purpose of this study to prove one technique or surgical variation over another but to outline the unique benefits of the femtosecond laser in cataract surgery from an experienced surgeon (since June 2011) in a single center with emphasis on the immediate visual outcomes and overall safety.
Experimental Procedure
The authors prospectively reviewed, from January 1, 2015 to December 31, 2017, a total of 2134 cases from one surgeon at one center. Primary emphasis was to evaluate phacoemulsification time in seconds (PT), ultrasound time in seconds (UT), and cumulative delivered energy in % per second (CDE) in the entire group and document differences between these groups. As a secondary object of this study the authors reviewed a subgroup of cases (n=1913) which were matched by Lens Opacification Classification System III. 20 Finally, 150 matched cases, from group two (n=1913) were performed prospectively and examined post operatively at three hours to compare vision.
Materials and Methods
Phacoemulsification, irrigation-aspiration parameters and femtosecond laser settings were standardized for each case. (Table 1) The phacoemulsification machine used was the same for every case (Model Infiniti; Alcon Laboratories, Inc., Fort Worth, TX, USA). A 0.9 mm mini-flared tip with continuous Ozil was used in all cases. The femtosecond laser used was the same for every case in which it was utilized (Model LenSx; Alcon Laboratories, Inc., Fort Worth, TX, USA) (Table 2). A six-cylinder and six-chop pattern was utilized in all cases. The same surgeon (KS) performed all cases using similar techniques in all cases. Topical proparacaine with monitored anesthesia care was provided in all cases. Viscoat® (sodium chondroitin sulphate and sodium hyaluronate) was utilized intraoperatively for protection of the cornea in all cases (Alcon Laboratories, Inc., Fort Worth, TX, USA). Provisc® (sodium hyaluronate) was utilized for lens implantation in all cases (Alcon Laboratories, Inc., Fort Worth, TX, USA).
Table 1. Phacoemulsification Settings| Irrigation | 95 cmH2O |
| Vacuum | 5mmHg (limit 360) |
| Torsional | 0% (limit 100) |
| Aspiration Rate | 0 cc/min (limit 36) |
| Capsule | Energy (uJ) | 6 | |
| Upper Depth (um) | 3564 | Reference Center | DP |
| Lower Depth (um) | 3986 | X Decentration (mm) | -0.624 |
| Delta Up (um) | 300 | Y Decentration (mm) | -0.331 |
| Delta Down (um) | 300 | Highest Energy (uJ) | 7 |
| Diameter (mm) | 5.3 | ||
| Lens | Highest Energy (uJ) | 7 | |
| Anterior Caps Depth (um) | 3515 | Reference Center | DP |
| Posterior Caps Depth (um) | 7472 | X Decentration (mm) | -0.624 |
| Chop Diameter (mm) | 5.2 | Y Decentration (mm) | -0.331 |
| Cylinder Diameter (mm) | 5.2 |
Results
The outcomes of Group 1 (n=2134) are summarized in Figure 1. The outcomes were reduced to compare the results for the femtosecond laser group (FS) versus the mechanical keratome group (CS). The average PT was 20.28 seconds in the femtosecond laser group (FS) and 33.12 seconds in the mechanical cataract (CE =standard) group (Figure 1). The average UT in the femtosecond group was 61.79 seconds and 68.87 seconds in the mechanical cataract or standard group (Figure 1). The p values comparing the FS subgroup for Group and the CS subgroup for Group 1 for PT, UT, and CDE were as follows: (0.001, 0.001, and 0.001). All p values showed statistical significance. In Group 1 (n=2134)the femtosecond laser was utilized for all cases (there was no preoperative case selection bias) including any and all ocular abnormalities such as trauma, pseudoexfoliation, posterior or anterior polar cataracts , patients on Tamsulosin (Flomax®) , small pupils, previous refractive surgery, Fuch’s corneal dystrophy, previous retinal surgery (including vitrectomy), and any cataract graded Lens Opacification Classification III NO4/NC4 or higher up to and including mature white cataracts. 20 Group 2 (n-1913) outcomes are summarized in Figure 2. Group 2 included a group of preoperatively case matched patients (n-1913). In this preoperatively matched by lens opacification Group 2 (n-1913), 869 patients underwent standard incisional cataract surgery (CS n-869) and 1044 patients underwent femtosecond assisted cataract surgery (FS n-1044). The average PT was 12.6 seconds in the femtosecond laser group (FS) and 33.12 seconds in the mechanical cataract (CE =standard) group (Figure 2). The average UT in the femtosecond group was 53.92 seconds and 67.87 seconds in the mechanical cataract or standard group (Figure 2). PT, UT and CDE were more noticeably reduced (PT 33.12 vs 12.6, UT 67.87 vs 53.922 and CDE 13 vs 8.329) when comparing results from the standard cataract surgery group (CS n-869) to the the femtosecond laser group (FS n-1044)in this matched lens opacity Group 2 compared to the results in Group 1 (unmatched cases).The p values comparing the FS subgroup to the CS subgroup for the PT, UT, and CDE in Group 2 were as follows: (0.001, 0.001, and 0.001). All these values show statistical significance.
Figure 1.Chart depicting the outcomes of Group 1 (unmatched lens group) comparing PT, UT, and CDE using FS versus CE technique.
Figure 2.Chart depicting the outcomes of Group 2 matched by lens opacity comparing PT, UT, and CDEin the FS (n-1044) versus CE (n-869) subgroups.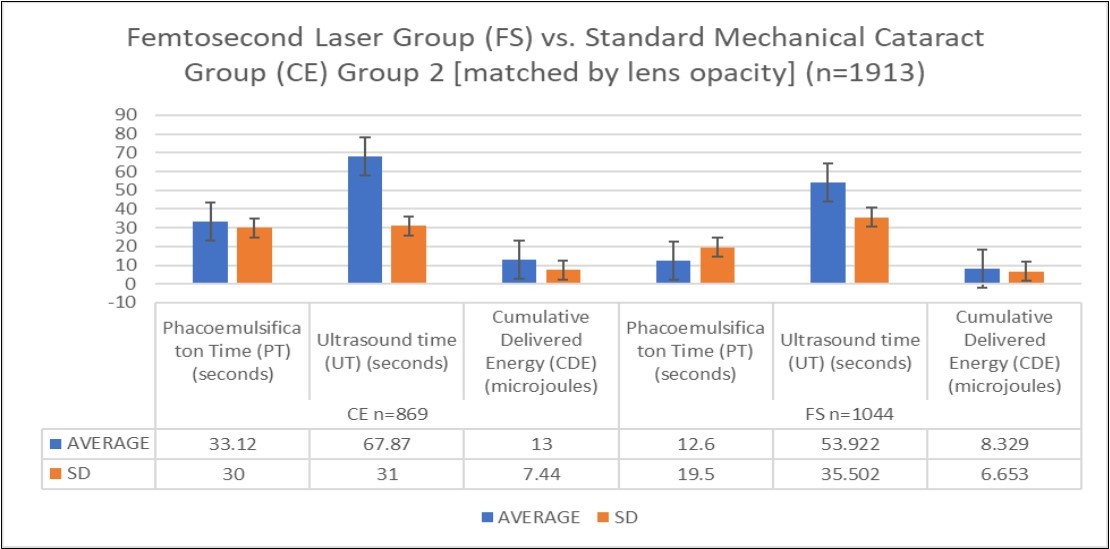
The data from both Group 1 (unmatched preoperatively) and Group 2 (matched by lens opacification) showed significant reductions in all parameters of PT, UT, and CDE when comparing the subgroups of femtosecond laser group (FS) to standard cataract surgery subgroups (CS). There were more noticeable differences (reductions in parameters) since the matched group (Group 2) and the unmatched group (Group 1) required small deviations in the intraoperative techniques requiring more surgical time.
The authors then reviewed a subset of 150 eyes prospectively from Group 2 (n-1913 case matched lens opacity group) who had visual acuity tested three hours after surgery. The visual acuity was performed during separate days of surgery performed by the same surgeon prospectively over one month. The visual acuity results are summarized in Figure 3. The average 3-hour uncorrected visual acuity in the femtosecond group was 0.64 (approximately 20/32) and 0.44 (approximately 20/50). These differences were statistically significant (p<0.001) (Figure 3). The authors observed that the reduced energy and time in the eye was positively correlated to the improved level of uncorrected vison at 3 hours after surgery.
Figure 3.Chart depicting the difference between FS and CE for 3-hour postoperative uncorrected visual acuity amongst a subset of 150 patients from Group 2 matched patients (n-1913).
Complications rates were also evaluated for Group 2 (matched cases n- 2134). The vitrectomy rate was 0.35% (3/869) in the mechanical (CS standard cataract) group and 0.16% (2/1265) in the femtosecond group (FS). . The overall vitrectomy rate for all cases was 0.23% (5/2134). There was one case of cystoid macular edema in the standard or mechanical cataract group (CS n-869), an incidence of 0.12% (1/869). This case included placement of an anterior chamber lens which developed subsequent cystoid macular edema. There was also one case of cystoid macular edema in the femtosecond group (FS n-1265), an incidence of 0.08% (1/1265). This was a patient who stopped their medications in the first postoperative week and failed to return for follow-up until 4 months postoperatively. Unique to the mechanical group (CE) was one case that required suturing of the wound (1/869), an incidence of 0.12% In the femtosecond laser group (FS n-1265), there were two cases that required residual retained lens fragments removal (2/1265), an incidence of 0.16%. Both of these cases required a return to surgery and involved only aspiration of the fragments (without vitrectomy and no other surgical procedures). There were no cases of endophthalmitis or other significant complications in either group.
Discussion
Rapid Improvement of Vision in the Immediate Postop Period
For surgeons that perform laser refractive and cataract surgery, safety and rapid outcomes are mainstay and expected. The difference between a patient seeing 20/30 in 3 hours versus 20/50 is noticeable to the patient and statistically significant as shown in Figure 3. As with other studies, this improved early vision difference did not persist at the 3-month visit. 17 Differing technique, such as the surgeon in this study tending to use epinuclear setting more often in the femtosecond laser group, lead to obvious reductions in overall energy released during surgery. All cases received the same postoperative medication regimens.
Surgical Time in the eye and Associated Complications
In addition to reduced phacoemulsification times, time spent overall in the eye was reduced. This reflects increased safety with regards to potential complications related to increased surgery time. Both groups had no incidence of endophthalmitis, but vitrectomy rates were higher in the mechanical group despite those cases including less of a complicated preoperative assessment. In the study by Abell, et al, complication rates were similar between those patients receiving femtosecond laser surgery versus conventional surgery alone. In fact, the author’s rate of vitrectomy in this study was 0.35% in the mechanical group versus 0.16% in the femtosecond laser group. These were similar when compared to that of Abell et al. (0.43% v 0.18%). 17 Scott et al. showed a similar reduction in vitrectomy rates favoring the femtosecond laser group. 21 One complication unique to the femtosecond laser group was retained lenticular fragments at 0.16%. Early perioperative intervention led to no further complications associated with this issue. Finally, although the sample size of 2134 is relatively small, cystoid macular edema rates overall was essentially contained to two cases in entire study. The single case of cystoid macular edema in the mechanical group was a complex case requiring an anterior chamber lens placement. The overall CME rate of 0.093% (2/2134) was lower when compared to the recently reported PREvention of Macular EDema after Cataract Study (PREMED) incidence of 1.5% CME for this group of combined treatment regimen of topical bromfenac and dexamethasone. In this study, all the patients received topical bromfenac and difluprednate ophthalmic and over 59% (1265/2134) of patients underwent femtosecond laser surgery. 22 Reduced energy could reduce the overall inflammatory component of surgical healing as reported previously and seen with this present study. 23
Economics
Our center averages 3.7 cases per hour when utilizing the femtosecond laser with a single surgeon. Surgeons report 4-5 cases per hour in similar environments with standard cataract surgery. (Personal Communications) Obviously, the cost of the laser, cost of disposables associated with the laser, the increased surgery operating room and operating room staff time is not comparable when evaluating the femtosecond laser assisted surgery compared to standard or mechanical surgery group. 9 However, the benefit of increased surgeon fees and reduced complications are a challenge to compare. What are the parameters used to determine if a incremental improvement in an already excellent surgical procedure make it “beneficial”. Unfortunately, decisions regarding costs must be made, and cutting corners in technology is one way to produce an outcome for the population as a whole. Tauber et al. continue to provide femtosecond laser cataract surgery to every patient who is a candidate, so the model is doable on a large scale. (Personal Communication-Providing femtosecond laser for all: The Mercy Hospital Model. Presented at the American College of Eye Surgeons, Aspen Colorado, 2017)
Patient Perception
Patient’s perceive lasers as part of surgery in a variety of fields. In this study, we did not perform a comparison of patient perceptions towards lasers. Patients do notice the difference when visual outcomes are statistically better at the 3-hour testing timeframe, but this is a challenge to measure. In our study, patients were statistically in favor to the femtosecond laser. 24. We also did not discuss potentially fewer visual aberrations and defects (rupture) when using the femtosecond laser to perform a capsulotomy when compared to continuous curvalinear capsulotomy (CCC) and other mechanical capsulotomies. Lee et al showed that the astigmatic change was more predictable in the femtosecond laser–assisted cataract surgery and internal aberrations, including total RMS, tilt, and RMS HOAs, were lower in the femtosecond group, and patients in that group were more satisfied. 18
Conclusion
The advantages and disadvantages of femtosecond laser assisted cataract surgery has been discussed at length in the literature. It really boils down to cost and time from a disadvantage standpoint. Is the extra time worth the benefits and are the added costs making a difference in terms of clinical outcomes? This paper illustrates the rapidity of recover with this technology. We also did not discuss or consider that post surgical patients returning to the work force in a timely fashion cannot be underestimated in the realm of “outcomes and benefits”. Safety is something a surgeon can never down play and this data supports the excellent safety profile added to cataract surgery, in a procedure that has already proven safe and effective.
The use of the femtosecond laser in cataract surgery will remain controversial, primarily related to time constraints, costs and overall economics. 9 In this single surgeon series from a single center, safety and outcomes favor femtosecond laser surgery in group matched settings. The surgeon in this series prefers to utilize the femtosecond laser in the more challenging cases secondary to these findings. The center utilized in this study has had access to the femtosecond laser since June 2011. There are currently seven surgeons that utilize this center, and they all vary on their use of the femtosecond laser in cataract surgery. For now, it will be a surgeon related choice coupled with the patients understanding of the procedure and of course their financial status. With time and improvement in technology, the authors believe it will become standard when it becomes more cost effective.
References
- 1.Nagy Z, Takacs A, Filkorn T, Sarayba M. (2009) Initial clinical evaluation of an intraocular femtosecond laser in cataract surgery. , J Refract Surg; 25, 1053-1060.
- 2.Nagy Z Z, Kranitz K, Takacs A I, Mihaltz K, Kovacs I et al. (2011) Comparison of intraocular lens decentration parameters after femtosecond and manual capsulotomies. , J Refract Surg; 27, 564-569.
- 3.Filkorn T, Kovacs I, Takacs A, Horvath E, Knorz M C et al. (2012) Comparison of IOL power calculation and refractive outcome after laser refractive cataract surgery with a femtosecond laser versus conventional phacoemulsification. , J Refract Surg; 28, 540-544.
- 4.Roberts T V, Sutton G, Lawless M A, Jindal-Bali S, Hodge C. (2011) Capsular block syndrome associated with femtosecond laser–assisted cataract surgery. , J Cataract Refract Surg; 37, 2068-2070.
- 5.Yeoh R.Hydrorupture of the posterior capsule in femtosecond laser (2012) cataract surgery [letter]. J Cataract Refract Surg; 38: 730; reply by TV Roberts. , G Sutton, MA Lawless, S Bali-Jindal, C Hodge,730
- 6.Bali S J, Hodge C, Lawless M, Roberts T V, Sutton G. (2012) Early experience with the femtosecond laser for cataract surgery. Ophthalmology ;. 119, 891-899.
- 7.Abell R G, Kerr N M, Vote B J. (2013) Femtosecond laser-assisted cataract surgery compared with conventional cataract surgery. , Clin Exp Ophthalmol; 41, 455-462.
- 8.Sutton G, Bali S J, Hodge C. (2013) Femtosecond cataract surgery: transitioning to laser cataract. , Curr Opin Ophthalmol; 24, 3-8.
- 9.Abell R G, Vote B J. (2014) Cost-effectiveness of femtosecond laser-assisted cataract surgery versus phacoemulsification cataract surgery. , Ophthalmology 121(1), 10-16.
- 10.Alió J L, Abdou A A, Puente A A, Zato M A, Nagy Z. (2014) Femtosecond laser cataract surgery: updates on technologies and outcomes. , J Refract Surg 30(6), 420-427.
- 11.Alió J L, Soria F, Abdou A A, Peña-García P, Fernández-Buenaga R et al. (2014) Comparative outcomes of bimanual MICS and 2.2-mm coaxial phacoemulsification assisted by femtosecond technology. , J Refract Surg 30(1), 34-40.
- 12.Alio J L, Soria F, Abdou A A. (2014) Femtosecond laser assisted cataract surgery followed by coaxial phacoemulsification or microincisional cataract surgery: differences and advantages. , Curr Opin Ophthalmol 25(1), 81-88.
- 13.Popovic M, Campos-Möller X, Schlenker M B, Ahmed. (2016) Efficacy and safety of femtosecond laser-assisted cataract surgery compared with manual cataract surgery: a meta-analysis of 14 567 eyes. , Ophthalmology 123(10), 2113-2126.
- 14.Nagy Z Z, Takacs A I, Filkorn T. (2014) Complications of femtosecond laser-assisted cataract surgery. , J Cataract Refract Surg 40.
- 15.Roberts T V, Lawless M, Bali S J, Hodge C, Sutton G. (2013) Surgical outcomes and safety of femtosecond laser cataract surgery; a prospective study of 1500 consecutive cases.Ophthalmology. 120, 227-233.
- 16.Hatch K M, Talamo J H. (2014) Laser-assisted cataract surgery: benefits and barriers. , Curr Opin Ophthalmol; 25, 54-61.
- 17.Abell R G, Darian-Smith E, Kan J B. (2015) Femtosecond laser–assisted cataract surgery versus standard phacoemulsification cataract surgery: Outcomes and safety in more than 4000 cases at a single center. , J Cataract Refract Surg; 41, 47-52.
- 18.Lee J A, Song W K, Kim J Y, Kim M J, Tchah H. (2018) Femtosecond laser-assisted cataract surgery versus conventional phacoemulsification: Refracitve and aberrometric outcomes with a diffractive multifocal intraocular lens.J Cataract Refract Surg.;. 45(1), 21-27.
- 19.Roberts H W, Wagh V K, Sullivan D L, Hidzheva P, Detesan D I et al. (2018) A randomized controlled trial comparing femtosecond laser-assisted cataract surgery versus conventional phacoemulsification surgery.J Cataract Refract Surg.;45(1):. 11-20.
- 20.Chylack L T, Wolfe J K, Singer D M, Leske M C, Bullimore M A et al. (1993) The lens opacification classification system III. , Arch Ophthalmol 111(6), 831-836.
- 21.Scott W J, Tauber S, Gessler J A, Ohly J G, Owsiak R R et al. (2016) Comparison of Vitreous Loss Rates Between Manual Phacoemulsification Cataract Surgery and Femtosecond Laser–Assisted Cataract Surgery. , J Cataract Ref Surg; 42(7), 1003-1008.
- 22.Nuijts R. (2017) PREMED study results presented at. XXXV congress of the ESCRS in Lisbon. EuroTimes .
