Abstract
Coronavirus Disease 2019 (COVID-19) placed significant pressure on global health systems, necessitating rapid and widespread immunization, especially among healthcare workers (HCWs). Despite being prioritized in immunization programs, variations in vaccine uptake among HCWs have been reported across different settings. This study aimed to investigate the predictors of COVID-19 vaccine uptake among HCWs in Kiambu County, Kenya. An analytical cross-sectional study design was employed, involving 112 HCWs sampled using stratified random sampling from Level 2 to Level 5 healthcare facilities. Data were collected through a pre-tested and validated 18-item questionnaire and analyzed using SPSS version 29.0. Statistical methods included descriptive analysis, chi-square tests, logistic regression, and ANOVA. The overall COVID-19 vaccine uptake was 88.9%. Significant predictors of uptake included age (p = 0.048), cadre (p = 0.015), and facility level (p = 0.031). Knowledge of COVID-19 vaccines emerged as the strongest predictor, with HCWs demonstrating good-to-excellent knowledge being 14.97 times more likely to be vaccinated (p < 0.001). Confidence in vaccine safety and effectiveness was also significantly associated with uptake (p < 0.001). Uptake was highest in Level 5 hospitals and lowest in dispensaries. The study reveals high vaccine uptake among HCWs in Kiambu County, but disparities persist due to individual and systemic factors. Strengthening vaccine education, institutional support, and deploying mobile vaccine education units in lower-level facilities could help close these gaps, offering practical strategies for improving HCW vaccine coverage in Kenya and other low- and middle-income countries.
Author Contributions
Academic Editor: Giuseppe Murdaca, Department of Internal Medicine-University of Genova, Genova, Italy
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2025 Edmond Muthee Waweru, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
The COVID-19 pandemic posed an unprecedented threat to global health systems, with healthcare workers (HCWs) at the frontline facing heightened exposure and operational strain. Vaccination quickly emerged as a key strategy for mitigating morbidity, mortality, and healthcare system overload1. Given their high risk and strategic role in pandemic response, HCWs were prioritized in national vaccination programs. However, vaccine uptake among HCWs has varied widely, influenced by individual perceptions, systemic barriers, and institutional dynamics 2.
Globally, studies have identified knowledge, confidence in vaccine safety, and professional cadre as important determinants of vaccine acceptance 3. In many cases, vaccine hesitancy among HCWs has stemmed from concerns about long-term side effects, misinformation, and limited trust in public health messaging. These issues are more pronounced in low- and middle-income countries (LMICs), where structural limitations and historical mistrust in government-led health initiatives remain prevalent 4
In Kenya, the Ministry of Health launched its COVID-19 vaccination campaign in March 2021, prioritizing HCWs and other essential workers. Despite this, national uptake varied, with Kiambu County—one of the most urbanized and densely populated counties—lacking localized evidence on HCW vaccine behavior 5. As a peri-urban county bordering Nairobi, Kiambu hosts a mix of high- and low-tier healthcare facilities, making it an ideal setting for examining regional disparities in vaccine uptake. Yet, there has been limited research on the specific predictors of vaccine acceptance among HCWs in this region.
International and regional studies suggest that both individual and system-level factors—such as age, cadre, vaccine literacy, peer influence, and institutional support—may significantly affect HCW vaccine decisions 6, 7. Within Kenya, a recent mixed-methods study identified lack of targeted information and poor access to structured educational campaigns as barriers to HCW vaccine uptake 8. These findings underscore the need for a localized, data-driven approach to understanding vaccine uptake patterns in Kiambu County.
This study therefore aimed to investigate the predictors of COVID-19 vaccine uptake among healthcare workers in Kiambu County. Specifically, it sought to determine the level of vaccine uptake, assess the influence of individual factors such as knowledge and demographics, and evaluate the role of health system determinants, including facility type and access. The following hypotheses were tested: (H₀₁) there is no significant relationship between individual-level factors and COVID-19 vaccine uptake among HCWs; and (H₀₂) there is no significant relationship between health system-level factors and vaccine uptake.
While the study provides critical insights, certain limitations must be acknowledged. The cross-sectional design restricts causal inference. Data were self-reported, introducing potential for response bias. The online mode of data collection may have excluded HCWs without digital access, and the sample was limited to Kiambu County, which may affect generalizability. Nonetheless, the study offers context-specific evidence to inform vaccine promotion strategies among healthcare providers in similar peri-urban LMIC settings.
Materials and Methods
This study adopted an analytical cross-sectional design to assess predictors of COVID-19 vaccine uptake among healthcare workers (HCWs) in Kiambu County, Kenya. The study population included doctors, nurses, clinical officers, pharmacists, laboratory personnel, and other cadres actively engaged in health service delivery during the COVID-19 vaccination rollout.
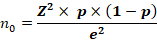
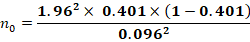
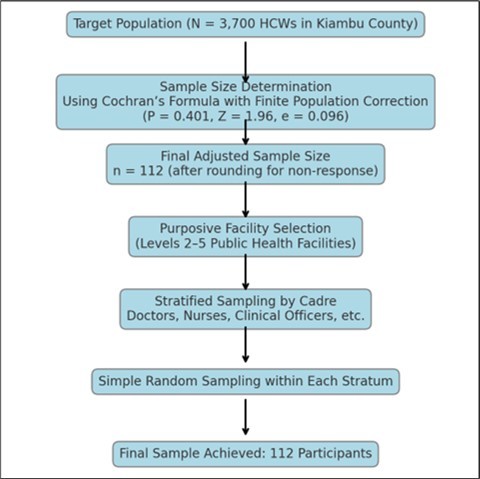
Using Cochran’s formula adjusted for a finite population (N = 3,700 HCWs in Kiambu County) 9, the minimum sample size was calculated and adjusted to 112 participants. The vaccination uptake rate of 40.1% from a comparable peri-urban setting (Kitengela) was used as the baseline proportion.
Kenya’s health system is structured into six levels under the Ministry of Health’s KHSSP and KEPH frameworks. Level 1 consists of community health services led by volunteers. Level 2 includes dispensaries offering basic outpatient care. Level 3 health centres provide outpatient, maternal, and limited inpatient services. Level 4, or sub-county hospitals, offer inpatient, surgical, and emergency care. Level 5 county referral hospitals provide specialized services and act as referral centers. Level 6 comprises national referral and teaching hospitals offering advanced care, training, and research. This study focused on healthcare facilities from Level 2 to Level 5 in Kiambu County.
A stratified random sampling technique was employed to ensure proportional representation across HCW cadres. First, purposive sampling was used to select eight public healthcare facilities spanning Levels 2 to 5, including Kiambu and Thika Level 5 hospitals. Within each facility, participants were randomly selected across cadres based on existing workforce proportions to reduce selection bias and improve generalizability within the county. The sample size was calculated using Cochran’s formula for proportions with finite population correction to ensure adequate statistical power and representativeness.
Cochran’s Formula :
Population size (N): 3,700
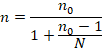
Application for Finite Population Correction (FPC) was done because the population is finite (N = 3,700). Hence, adjustment was done for n0:
This gave a final sample size of ~98, but rounding up for non-response or practicality was done to 112. Figure 1
Data were collected using a structured, 18-item online questionnaire, which included closed-ended and Likert-scale items assessing demographics, vaccine knowledge, attitudes, uptake, and health system influences. The tool was developed from literature and existing validated instruments, including components from 10.
A pretest involving 12 HCWs from Kitengela was conducted to refine clarity and structure. Following the pretest, modifications were made to improve readability and eliminate leading questions. The reliability of the knowledge subscale was measured using Cronbach’s alpha, yielding a score of 0.85, indicating strong internal consistency. Content validity was assured through expert review by public health and immunization specialists, and face validity was achieved through pretesting with frontline HCWs.
Data were entered and analyzed using SPSS version 29.0. Descriptive statistics (means, frequencies, percentages) were computed for demographic variables. Bivariate associations were tested using Chi-square tests for categorical variables and independent samples t-tests or ANOVA for continuous variables like confidence scores.
Logistic regression was employed to determine predictors of vaccine uptake, particularly focusing on knowledge levels, professional cadre, and facility level. Significance was set at p < 0.05.
The study received ethical approval from the Kenyatta University Research Ethics and Review Committee, and permissions were obtained from the National Commission for Science, Technology, and Innovation (NACOSTI) as well as the Kiambu County Health Department.
Participants were recruited voluntarily and provided informed consent electronically. Confidentiality and anonymity were ensured through coded responses, secure data storage, and limited access to research personnel. HCWs on leave, unavailable during data collection, or serving in non-clinical support roles were excluded. Data collection was conducted via a secure online platform, primarily through WhatsApp, which is commonly used by HCWs in Kenya.
Results
The socio-demographic profile of respondents is presented in Table 1. The majority were female (54.5%), and most participants were aged 31-40 years (33.33%). In terms of marital status, single HCWs comprised 66.96% of the sample.
Table 1. Socio-demographic characteristics of the study participants| Variable | Categories | Frequency (n=112) | Percentage (%) |
|---|---|---|---|
| Gender | Male | 51 | 45.5 |
| Female | 61 | 54.5 | |
| Age Group (years) | 18 - 30 | 19 | 16.67 |
| 31 - 40 | 37 | 33.33 | |
| 41 - 50 | 31 | 27.78 | |
| 51 - 60 | 19 | 16.67 | |
| 61+ | 6 | 5.56 | |
| Marital Status | Single | 75 | 66.96 |
| Married | 26 | 23.21 | |
| Widowed | 2 | 1.78 | |
| Divorced/Separated | 9 | 8.04 |
A logistic regression analysis confirmed that HCWs with good-to-excellent knowledge of COVID-19 vaccines were 14.97 times more likely to be vaccinated (OR = 14.97, 95% CI = 5.35 – 39.20, p < 0.001) Table 2.
Table 2. Logistic Regression Analysis: Knowledge as a Predictor of Uptake| Knowledge Level | Vaccinated | Not Vaccinated | OR | 95% CI | p-value |
|---|---|---|---|---|---|
| Poor/Fair (Reference) | 33.0% | 67.0% | 1.00 | Reference | - |
| Good/Excellent | 87.9% | 12.1% | 14.97 | 5.35 – 39.20 | < 0.001 |
This multivariable logistic regression model examines predictors of COVID-19 vaccine uptake using knowledge level, facility type, and professional cadre as explanatory variables Table 3.
Table 3. Multivariable logistic regression of vaccine uptake| Predictor | Coefficient (β) | Std. Error | z-value | p-value | 95% CI (Lower–Upper) |
|---|---|---|---|---|---|
| Knowledge Level | -0.73 | 0.38 | -1.92 | <0.001 | -1.48 – 0.01 |
| Facility Type | 0.04 | 0.26 | 0.17 | 0.031 | -0.47 – 0.56 |
| Cadre | -0.29 | 0.20 | -1.46 | 0.015 | -0.69 – 0.10 |
Discussion
This study assessed the predictors of COVID-19 vaccine uptake among healthcare workers (HCWs) in Kiambu County, Kenya, and established that while the overall uptake was high at 88.9%, there were significant disparities based on cadre, facility level, and knowledge. The strongest predictor of vaccine uptake was knowledge of COVID-19 vaccines, with HCWs possessing good-to-excellent knowledge being nearly fifteen times more likely to be vaccinated than those with limited understanding. Uptake was highest among staff in Level 5 hospitals and lowest in Level 2 dispensaries, highlighting a tiered disparity in access, exposure, and institutional reinforcement. These findings suggest that despite the availability of vaccines, uptake is still heavily influenced by informational, systemic, and contextual factors.
When viewed alongside similar African studies, the results mirror regional patterns in HCW vaccine behavior. In South Africa, 4 reported that vaccine acceptance among HCWs was highest in institutions with strong internal communication and consistent public health messaging, reinforcing the current study’s finding that Level 5 hospitals had superior uptake due to structured governance and information access. In Nigeria, 6 similarly found that HCWs with strong knowledge and peer engagement were significantly more likely to accept vaccination, highlighting the role of collegial influence and institutional culture in driving positive behavior. A comparable pattern was noted in Tanzania by 11, where HCWs in rural and low-tier settings were more hesitant due to inconsistent messaging, misinformation, and lack of professional advocacy.
In Ghana, 12 emphasized that perceived risk, professional cadre, and institutional endorsement were critical in vaccine decision-making. This resonates with our findings, where cadre differences were significant, with medical officers and nurses demonstrating higher uptake compared to support staff. Working across Kenya and Tanzania8, showed that vaccine confidence was often rooted in how well facilities managed staff engagement and education, again affirming the present study’s conclusion that information access and institutional reinforcement are crucial determinants of uptake. Collectively, these regional findings contextualize the present study within a broader continental discourse, suggesting that while vaccine availability is necessary, it is not sufficient without accompanying systemic and informational support.
One of the most important insights from this study is the disproportionate hesitancy among HCWs stationed in lower-tier facilities. With Level 2 dispensaries reporting uptake as low as 74.2%, the data point to a worrying gap in equitable protection of frontline health workers. It is plausible that such facilities, often more remote and under-resourced, receive less direct engagement from policy implementers and fewer opportunities for structured training. Speculatively, these environments may also be more susceptible to misinformation, especially where digital access is low and professional isolation is high. The knowledge gap becomes both a symptom and a driver of hesitancy, as HCWs without regular exposure to trusted sources may default to skepticism or defer vaccination altogether.
These disparities have broader implications for health systems resilience and equity. Unequal uptake among HCWs can translate into uneven service delivery, with unvaccinated staff more vulnerable to infection, absence, and even death. Furthermore, HCWs serve as key influencers in community health behavior. If confidence and uptake among HCWs in lower-tier facilities are low, this could negatively influence community perceptions and reduce overall vaccine coverage. As such, HCW vaccine uptake is not only a workforce protection issue but also a barometer of public trust in the health system. 13 Similar local findings have warned that HCWs with poor vaccine literacy may inadvertently become vectors of misinformation, undermining public health campaigns and fueling hesitancy in the communities they serve.
From a systems perspective, the data indicate that top-down strategies alone may be insufficient. While national policy frameworks and supply logistics have facilitated overall access, the subtler, context-driven components—knowledge transfer, peer influence, and institutional culture—are often under-addressed. This study demonstrates that HCWs respond not only to policy mandates but also to how those mandates are delivered and reinforced within their work environment. The implication here is that policy execution must be as adaptive and decentralized as possible, engaging HCWs at their point of practice and respecting the variability in their professional experiences and facility contexts. Such an approach would mirror suggestions by 8, who advocated for decentralized, peer-led training in low-resource settings to enhance vaccine literacy.
The potential significance of this study lies in its applicability for designing smarter, more targeted vaccine strategies in LMICs. The results suggest that with adequate knowledge and institutional reinforcement, high uptake is achievable even in diverse settings. Kenya’s Ministry of Health can leverage this insight to develop cadre-specific and facility-level interventions that bridge the uptake gap. These may include on-site vaccine literacy sessions, integration of vaccine education into continuous professional development (CPD), and mobilization of peer champions within facilities. The evidence points to the need for a multipronged communication strategy, one that not only informs but also reassures and empowers HCWs to make confident, informed choices.
Policy implications from this study are both immediate and far-reaching. The Ministry of Health should consider embedding HCW vaccine uptake indicators into its national health performance monitoring systems, disaggregated by facility level and professional cadre. Such granularity would allow policymakers to track disparities and deploy targeted interventions. Regular vaccine knowledge audits should also be institutionalized, particularly in counties or facilities with persistently low uptake, and findings should inform tailored education campaigns. Additionally, national CPD frameworks should mandate immunization modules, ideally co-developed with universities and professional councils, to ensure consistency and accreditation.
Resource allocation strategies may also need revision. Facilities that demonstrate consistent vaccine hesitancy may require increased funding for staff training, supervisory visits, and engagement with health promotion officers. Linking HCW vaccine uptake to performance-based incentives or facility accreditation metrics could further encourage compliance and institutional ownership. Moreover, investment in digital health education platforms and mobile outreach units would enhance reach, especially to HCWs in remote or underserved areas. These strategies align with Kenya’s broader Universal Health Coverage (UHC) goals by protecting the workforce essential to delivering equitable, quality care.
While the overall COVID-19 vaccine uptake among HCWs in Kiambu County is encouraging, this study surfaces critical disparities that must be addressed for the program to be truly equitable and effective. The association of uptake with cadre, knowledge, and facility level is consistent with findings across Africa, reinforcing the argument that vaccine programs must go beyond supply logistics to include structured education, peer influence, and localized policy enforcement. The Ministry of Health is well positioned to act on these insights, institutionalizing vaccine education, embedding disaggregated monitoring into national systems, and mobilizing resources to support low-performing facilities. By doing so, Kenya can safeguard its healthcare workforce and build a more resilient health system prepared for future public health emergencies.
Conclusion
This study identified age, professional cadre, facility level, and vaccine knowledge as key predictors of COVID-19 vaccine uptake among HCWs in Kiambu County. While uptake was relatively high, addressing persistent hesitancy through targeted education, equitable access, and strong institutional support is essential for maintaining HCW protection in current and future public health emergencies.
Conflict of Interest
The author declares no conflicts of interest.
Affiliations
Department of Family Medicine, Community Health and Epidemiology, School of Health Sciences, Kenyatta University, Nairobi, Kenya
Acknowledgements
The author acknowledges Prof. Wanyoro and Dr. Tembu for their mentorship, the healthcare workers who participated, and the research and ethics bodies that provided support and approvals for this study. The study was conducted with full ethical clearance from the Kenyatta University Ethics Review Committee.
References
- 1.BAS Machado, KVS Hodel, LMDS Fonseca, Pires V C, LAB Mascarenhas et al. (2022) . The Importance of Vaccination in the Context of the COVID-19 Pandemic: A Brief Update Regarding the Use of Vaccines , Vaccines. MDPI; 10.
- 2.Desye B. (2022) Prevalence and Determinants of COVID-19 Vaccine Acceptance Among Healthcare Workers: A Systematic Review. 10.
- 3.Kaplan R M, Milstein A. (2021) Influence of a COVID-19 vaccine’s effectiveness and safety profile on vaccination acceptance. 118-10.
- 4.George G, Nota P B, Strauss M, Lansdell E, Peters R et al. (2023) . Understanding COVID-19 Vaccine Hesitancy among Healthcare Workers in South Africa. Vaccines , (Basel) 1, 11-2.
- 5.Kenya Ministry (2022) of Health. Ministry of Health Kenya COVID-19 vaccination program-Daily Situation Report: Current Status Total doses Administered.
- 6.Nnaemeka V C, Onwe R O, Ekwedike A L, Oyedele O E, Tsiterimam T S et al. (2022) . Predictors of COVID-19 Vaccine Acceptance among Healthcare Workers in Nigeria. Vaccines , (Basel) 1, 10-10.
- 7.Ghare F, Meckawy R, Moore M, Lomazzi M. (2023) . Determinants of Acceptance of COVID-19 Vaccination in Healthcare and Public Health Professionals: A Review., Vaccines. MDPI; 11.
- 8.Binyaruka P, Mtenga S M, Mashasi I, Karugu C H, Mohamed S F et al. (2023) Factors associated with COVID-19 vaccine uptake among people with type 2 diabetes in Kenya and Tanzania: a mixed-methods study. , BMJ Open; 13(12).
- 9.Kenya Ministryof Health. Kenya Health Workforce Report: Contact Information [Internet]. Available from: http://www.health.go.ke.
- 10.Islam M S, Siddique A B, Akter R, Tasnim R, MSH Sujan et al. (2021) Knowledge, attitudes and perceptions towards COVID-19 vaccinations: a cross-sectional community survey in Bangladesh. BMC Public Health. 1, 21-1.
- 11.Gadbois E A, Brazier J F, Meehan A, Madrigal C, White E M et al. (2023) COVID-19 Vaccination Among Skilled Nursing Facility Staff: Challenges and Strategies Identified by Administrators. Medical Care Research and Review. 80(6), 608-18.