New Classification for Bifurcated Mandibular Neural Canal
Abstract
Objectives
To analyze the occurrence rate of bifurcated mandibular canal (BMC) by cone beam CT(CBCT) and summarise a new classification for further clinical work and academic communication.
Method
Randomly collected the CBCT images of 350 adult patients. Firstly, we analysed and summarized the BMCs into four types by the position of bifurcation point in the mandible. Second, we did statistics about occurrence. Then we have measured three kinds of distance of Type I and Type II. At last, we compared the advantages and disadvantages about different classifications.
Results
Among these 350 patients, we found 110 adult people with BMC which indicated the occurrence rate of BMC was 31.43%. The most common type was Type I, especially Type IB, and the least was Type III. Vertical distance between the apex of the second molar, the third molar and mandibular canal are 4.36±2.51 mm and 2.45±2.23 mm. Distance from the apex of two molars to the bifurcated spot are 15.87±6.82mm and 9.32±5.37mm. And the distance between the apex and retromolar foramen in Type I are 22.19±5.97mm and 15.82±4.68mm.
Conclusion
Comparing with former typing theory, we summarized a new classification which is simpler and more convenient, which should attach scholars’ attention to BMC during clinical work.
Author Contributions
Academic Editor: Yi Zhang, Beijing University of Chinese Medicine.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2022 Xiang Wang, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
In our dental clinical work, some patients have bleeding of unknown etiology, or neural symptoms of the mandibular nerve after alveolus surgeries, implantation, or sagittal split ramus osteotomy/bilateral sagittal split ramus osteotomy (SSRO/BSSRO). In exploring the causes of these symptoms, many scholars have found that the mandibular nerve canal has variations at different positions, rather than being a single canal.
Conventional theory described the mandibular canal (MC) as a cortical bone canal located between the cancellous bone of the mandible that travels inferoanteriorly in the mandibular ramus and almost horizontally forward in the body1. The small duct can stretch into each alveoli, providing a passage for the inferior alveolar nerve and vessels. The MC is divided into two parts at the mental foramen areas: the thicker one will become mental canal, and the thinner one will continue to form the incisive canal. Significant nerves and vessels run throughout both of them 2, 3, 4. Traditional views also point that MC is a single canal at mandible without branches. However, a large number of scholar state bifid and even trifid mandibular canals in their related work depending on the progressive radiologic technology 5, 6, 7, 8, 9, 10, 11, 12.
After these reports, more scholars have found it important to use other methods to research the variation of the mandibular canal, such as autopsy, histopathology, and imaging modalities (e.g., panoramic radiographs, cone beam computed tomography (CBCT), and spiral CT)5, 12, 13, 14. According to the results of the methods used, it has been confirmed that the mandibular canals are myelinated nerves, veins, and arterioles. The earliest scholars used panoramic radiographs to observe the variation, which indicated that the occurrence rate of variation was 0.038% to 1.98%12, 15, 16, 17, 18. With the widespread use of CBCT, a considerable number of scholars take advantage of the three-dimensional (3D) imaging to observe these variations more directly, making the occurrence rate as high as 10.2% to 66.5%5, 13, 19, 20, 21.
These values were sufficient to demonstrate that the bifurcated mandibular canal is not unusual. Zhang 22made a research about bifid variations of the mandibular canal of 1000 Northern Chinese patients by CBCT, which provide a more appropriately imagological way to do research on the anatomical variation of mandibular canal. Some researchers pointed out some theory of classifications about BMC among some their features and observation methods: Nortje23, R.P. Langlais et al24made correlative work by panoramic radiographs; Naitoh’s theory by using CBCT to classify the bifid mandibular canals was more widely accepted 21. Compared with the former inspection methods, CBCT give us more accurate way to study BMC. However, all these common theories are qualitative, which are limited by development of radiology and lack of specific evidence for clinical work.
As a result, we aimed to perform a research study on the structural variation of the mandibular neural canal by CBCT and, thus, pointed a constant symbol for classification and summed up a more comprehensive, yet simple, quantitative and practical typing theory for the bifurcated mandibular canals, to make clinical work and academic communication easier.
Material and Method
Material
The CBCT data of 350 patients aged 18 to70 years were randomly collected from the Xiangya Stomatological Hospital of Central South University between December 2012 and July 2017. Written informed consent was obtained from each participant. The study was approved by the Ethical Committee of Xiangya Stomatological Hospital of Central South University, approval number 20190033.
Sampling for Subject
Given the low prevalence of head and neck cancers which involve the skull base, we set
Inclusion criteria
a. Patients 18 to 70 years of age with complete images of the mandibular canal from the mandibular foramen to the mental foramen.
b. The mandible is integrated without obvious absorption, and the direction of the mandibular canal is not affected by the fracture line.
c. The image of mandibular foramen is intact and clear.
Exclusion criteria
a. CBCT image is blurred or there is interference in the observation area.
b. Mandible lesions (e.g., cyst, tumor, infection, severe osteoporosis) and other lesions that can obstruct observation.
c. After mandibular surgery, as the fracture line affects the direction of the mandibular canal, segmental resection, and SSRO.
Method
CBCT scanning: All the images used in this study were collected by the same CBCT scanner (PLANMECA), and all patients were imaged according to the standard process. Finally, the image data were stored in the PLANMECA Romexis software system.
Reading Images
In a quiet workspace, well-trained researchers adjusted the contrast images with software to make the bone structure clear and easy to define. Images were read twice with a 3-week interval between readings.
The second reading process was somewhat different: the researchers adjusted the sagittal images to make the lower edge of the mandible parallel to ground, then: (1) a horizontal line was made parallel to the lower edge of the mandible (Figure 1, grey line); (2) a tangent line was made along with the front edge of the mandibular ramus (Figure 1, green line), which intersects with the upper edge of the mandibular body (Figure 1, red circle); (3) a line across the intersection was made vertical to the line in (1) (Figure 1, yellow line). We defined the following: the bifurcation that appears in front of this vertical line (yellow line) is classified into mandibular body area, whereas the bifurcation that appears behind it is the mandibular ramus area (Figure 1). The classification of each type depends on the starting point of the bifurcation. Details are provided in Table 1.
Table 1. New classification of bifurcated mandibular canal| I | IA | A bifurcation at the mandibular ramus and the retromolar foramen has been formed. (Fig. 2A,B; Note 1) |
| IB | A bifurcation at the mandibular ramus and the retromolar foramen has not been formed. (Fig. 2C) | |
| II | Bifurcations at the mandibular body. (Fig. 2D) | |
| III | Bifurcations exist both at the mandibular body and the mandibular ramus on one side. (Fig. 2E; Note 2) | |
| IV | Other circumstances (e.g., trigeminal nerve canal or multi-canal derived from different origins) (Fig. 2F) | |
Figure 1.Image-reading position. (1) a horizontal line was made parallel to the lower edge of the mandible (grey line); (2) a tangent line of the front edge of the mandibular ramus (green line), which intersects with the upper edge of the mandibular body (Fig. 1, red circle); (3) a line across the intersection was made vertical to the line in (1) (Fig. 1, yellow line). We defined the following: the bifurcation that appears in front of this vertical line (yellow line) is classified into mandibular body area, whereas the bifurcation that appears behind it is the mandibular ramus area (Fig. 1).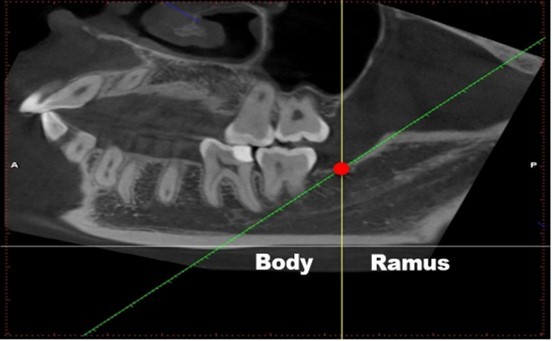
Results
New Classification of BMC
According to our rules, we divided BMC into four types. Type IA was bifurcations at the mandibular ramus, and retromolar foramen has been formed. Type IB was bifurcations at the mandibular ramus, and retromolar foramen has not been formed. We took those bifurcations at mandibular body as Type II. Type III was for bifurcations exist both at the mandibular body and the mandibular ramus on one side. Type IV for other circumstances. Details as following in Table 1 and Figure 2
*Note 1: If there are several branches at one side of the mandibular ramus at the same time,we add total numbers before the type and specific amount of subclass on the bottom right (e.g., 2IA, 3IA2B1). If the bifurcation point is exactly on the boundary of the body and ramus, we identify it as Type I.
*Note 2: If there are several branches, the number before the type represents the total amount, and the label at the top right shows the number of branches at the mandibular ramus; the label at the bottom right shows the number of branches at the mandibular body
Figure 2.New classification of BMC: The red arrow points to the bifurcations, and the yellow arrow points to the mandibular canal. (A) Type IA: Bifurcations at the mandibular ramus, and retromolar foramen has been formed. (B) Type IB: Bifurcations at the mandibular ramus, and retromolar foramen has not been formed. (C) Type II: Bifurcations at the mandibular body. (D)-(F) Type III: Bifurcations exist both at the mandibular body and the mandibular ramus on one side. (G) Type IV: Other circumstances.
Incidence Rate of BMC
Among the 350 patients in our study (120 males and 230 females), we found 110 patients with BMC, for an occurrence rate of 31.43%. Of these, 32 were males (26.67%) and 78 were females (33.91%) (Table 2.1). Besides, we also summed up the amount of different position, and the appearance of unilateral or bilateral BMCs. According to the result of χ2test, there was no statistically significant difference (Table 2.1 p= 0.183>0.05, Table 2.2 p=0.097>0.05, Tab 2.3 p=0.562>0.05). From all 700 sides of mandible, bifurcations occurred on 133 sides, as follows: 103 sides of Type I(14.71%);27 sides of IA(3.86%)and 76 sides of IB(10.86%);18 sides of Type II(2.57%);5 sides of Type III(0.71%);and 7 sides of Type IV(1.00%)(Tab.3). As shown in Table 2, Yes indicates a mandibular canal with bifurcations; No indicates a mandibular canal without bifurcations. As the result we can conclude that Type I is the most common one and IB for the subtype which can remind that we need to pay more attention on the bifurcation happened at mandibular ramus in our clinical work. Table 3
Table 2. 1. 350 samples of bifurcations in male and female mandibular canals| Yes | No | Amount | Incidence rate (%) | |
| Male | 32 | 88 | 120 | 26.67 |
| Female | 78 | 152 | 230 | 33.91 |
| Amount | 110 | 240 | 350 | 31.43 |
| Left | Right | Total | |
| Male | 13 | 25 | 38 |
| Female | 46 | 49 | 95 |
| Total | 59 | 74 | 133 |
| Unilateral | Bilateral | Total | |
| Male | 31 | 7 | 38 |
| Female | 78 | 17 | 95 |
| Total | 109 | 24 | 133 |
| Male | Female | Amount | Incidence rate (%) | ||
| I | IA | 7 | 20 | 27 | 3.86 14.71 |
| IB | 24 | 52 | 76 | 10.86 | |
| II | 5 | 13 | 18 | 2.57 | |
| III | 0 | 5 | 5 | 0.71 | |
| IV | 2 | 5 | 7 | 1.00 | |
| Amount | 38 | 95 | 133 | 19.00 | |
The Distance between Apex of Molars and Mandibular Canal
In our study, we measured the distance between apex of that two molars and BMCs. The second and third molar are closely related to oral maxillofacial surgery and implant surgery. Besides, these two molars are adjoined with the spot we formulated. In Table 4, we recorded the vertical distance between the apex of the second molar, the third molar and mandibular canal are 4.36±2.51 mm and 2.45±2.23 mm. The distance from the apex of the second molar, the third molar to the bifurcated spot are 15.87±6.82mm and 9.32±5.37mm. And, the distance between the apex of the second molar, the third molar and retromolar foramen in Type I are 22.19±5.97mm and 15.82±4.68mm. Because of the loss of the third molar, it results in the difference in the amount of samples. We should operate in this safe range of distance to avoid damaging mandibular nerves and vessels.
Table 4. Distance between two molar and anatomic site in Type I and Type II(mean ±SD)| Vertical distance (mm) | Bifurcated site(mm) | Retromolar foramen(mm) | |
| The second molar | 4.36±2.51 | 15.87±6.82 | 22.19±5.97 |
| The third molar | 2.45±2.23 | 9.32±5.37 | 15.82±4.68 |
Difference Between Four Theories
Details in Table 5.
Table 5. Difference between four theories| Methods | Basis of classification | Tool | Dimensions of image(2D/3D) | Category | Comprehensive coverage | Measured data | Incidence rate |
| Nortje et al. | The height of the mandibular canal in the mandible. | Orthopantomography | 2D | 4 | Position | None | 46.7% (1685/3612)Male:48.9%Female:45.7% |
| Langlais et al. | Unilateral bifurcation or bilateral and the relationship of convergence between bifurcation and the canal. | Orthopantomography | 2D | 4 | Unilateral or bilateral | none | Male:39%;Female: 61% |
| Naitoh et al. | Directions of the canal. | CBCT | 3D | 4 | Direction | The length of BMC: I:14.8; II:8.9; III:8.6; IV:1.6 | 65% (125) |
Discussion
Difference Between the Classification Theories
In nowadays, the most commonly admitted definition of BMC is to find the triangular “osseous inland” which is formed by the intersection of two pipes in panoramic radiographs and the vertex of the triangle is the starting point of the bifurcation of the mandibular canal. As early as 1977, Nortje et al. classified BMC according to the position of the bifurcations in the mandibular body23, this is the method that is earlier and more classic, laying the foundation for the follow-up. In 1985, R.P. Langlais et al. set up more specific theory based on the earlier scholars24. However, the two-dimensional analyzed method limited the observing and classifying the bifurcated mandibular canal. Besides, their method of classification is a little cumbersome for implication. Besides, their method of classification is a little cumbersome for implication. With the adventure of CBCT, Naitoh set up a new classification which could be more convenient to find the BMC21. It is more exhaustive and comprehensive than those previous methods with panoramic radiographs, such as its definition for buccal-lingual canal. This theory is more detailed and emphasizes the relationship with molars. But it cannot fully reflect the location of BMC, such as type 3, type 4. In addition, it is hard to accurately describe the existence of multiple canals and other complicated situations on one side.
At present, different scholars use different classification criteria which may result in many understandings of the classification methods and lead to inconsistent research results. Observers have different levels of understanding of the anatomical variation, and ignore to make the mutual verification of sagittal, coronal, and cross-section, all these can cause different results about the same image, even for the same classification criteria, various types of results may be inconsistent. Besides, the anatomical variations of the mandibular canal in different regions and different races may be inherently various. It may have relationship with congenital variations, lifestyle, chewing habit of some people. Further research is needed to verify whether these habits will lead to different occurrence rates of anatomical variation of mandibular canal.
The Advantages of our Classification Theory
At present, scholars use different classification criteria for BMC because of no consolidated standard, which may result in many inconsistent research results. Based on the explicitly defined the boundary of mandibular body and ramus, we made a reclassification of the BMC, and this improved method will help to guide future development of surgery. The classification can record the amount of multi-canal on one side, which is also more comprehensive and useful for other complicated situations. Also, we measured distances between root and inferior alveolar nerve canal and showed the sutures in detail, which can precisely guide surgical correction. Therefore, our method can supply a profound clinical significance for the mandible operation and it is easier for training and academic communication. Furthermore, we pointed a constant site and position for scholars to study BMC, which is stable for different population and more objective for measured data and clinical application.
Nevertheless, we only described the location, amount and other complicated conditions of the bifurcated mandibular canal. But our classification still has limitation in reflecting the general trend of the BMC and information about distance.
Clinical Implication of BMC
Block Anesthesia and Dental Extraction of the Mandibular Impacted Molar
The inferior alveolar nerve block anesthesia is very important for the dental extraction in our clinical operation. However, because of the improper operation and the BMC the success rate of block anesthesia of inferior alveolar nerve is 82%-91%25,26. Therefore, scholars aimed to the study of the anatomy and pathology of the mandibular bifurcation 1,8,12,27,28,29. Some research suggested the mandibular impacted teeth are closely related to the mandibular canal and its branches. Not only can Yamada30 find the incidence rate of BMC reaching to 94.6%, but 54.8% branches contact with the third molar. In another classify method, they categorized into 5 groups about the relationship between bifurcations of mandibular canal and the third molar31. But different methods to classify the relationship will have different result, which the outcomes from 28% to 94.6%32. For all this, the common bifurcate position of mandibular canal located around the retromolar pad. This is why the ineffective block anesthesia and bleeding appeared in clinical.
In our study, we pay attention to the precision measurement of distance between BMC to molar apical foramen. Our results showed that the average vertical distance from the second molar and third molar to BMC is only 4.36±2.51mm and 2.45±2.23mm. Meanwhile the bifurcated site to the root tips is less than 9mm. That means the blood supply and nerve distribution of molars were upper branch of BMC. This may explain why only a percentage of patients presented ineffective block anesthesia and bleeding even though they all have the same treatment. Therefore, we need to take a CBCT scan for further diagnose and to be gentle during extraction with the BMC patients in clinical practice.
Applied to Implantology
Implants denture have been normally accepted by clinicians and patients for their excellent ability to restore occlusion and safety for the adjacent teeth. However, each doctor has to consider the trend of MC; otherwise, it will be injured when implant surgery occurs in the mandibular molar and the premolar region. The most important clinical implication of BMC in implantology is to attract the attention of the majority of doctor in implant work. During daily clinical work, most implanters focus on the damage to the mandibular canal rather than bifurcation at mandibular body. What's more,Accurate localisation of mandibular canals in lower jaws is important in dental implantology, in which the implant position and dimensions are currently determined manually from 3D CT images by medical experts to avoid damaging the mandibular nerve inside the canal33. In this study, the incidence rate of Type II and Type III bifurcation at mandibular body are respectively 2.57% and 0.71%. Besides, vertical distance between the apex of the second molar, and mandibular canal is only 4.36±2.51 mm and distance from the apex of the second molar to the bifurcated spot are 15.87±6.82mm. The direction and depth of implant should follow the guidance of CBCT. This suggests that we must pay attention to these bifurcation at mandibular body. For some unexplained sense disorder, it may be related to injury or compression of BMC.
Applied to SSRO and RIF of Mandible Fracture
An important complication of sagittal split ramus osteotomy (SSRO) and rigid internal fixation (RIF) of mandible fracture is damage to the inferior alveolar nerve and blood vessels. Using a surgical template for mandibular angle osteotomy can effectively reduce those injuries, thus improving the safety and effectiveness of the surgery, which requires an accurate preoperative osteotomy design and an accurate estimate of the path of the mandibular neural tube branches34.In this study, Type I account for 14.71% and Type III for 0.71%, which suggests that there is a high risk of intraoperative injury. In other words, the symptoms of neurological disorders after surgery may be concerned with the damage of bifurcation at mandibular ramus.
Conclusion
In summary, we retrospectively studied the anatomical variation of the mandibular neural canal by CBCT and summed up a more comprehensive, simple, and practical classification for BMC, which can make clinical work and academic communication easier. The most common is Type I, especially Type IB, and the least is Type III. Finally, it is important for clinicians to identify this anatomical variation in extraction of mandibular third molar, block anesthesia of inferior alveolar nerve, mandibular molar implantation, and SSRO. Clinician should use CBCT to identify this structural variation in the risky area, which has important clinical implication for reducing complications.
Acknowledgements
This work has been supported by, the National Natural Science Foundation of China (81800952), the Natural Science Foundation of Hunan Province, China(2021JJ30987),Hunan Provincial Science and Technology Department(2018SK51002).The authors deny any conflicts of interest.
References
- 1.Schejtman R, Devoto F, Arias N. (1967) The origin and distribution of the elements of the human mandibular retromolar canal. Arch Oral Biol. 12, 1261-1268.
- 2.Jablonski N, Cheng C, Cheng L, Cheung H. (1985) Unusual origins of the buccal and mylohyoid nerves. Oral surgery, oral medicine, oral pathology and oral radiology. 60, 487-488.
- 3.Claeys V, Wackens G. (2005) Bifid mandibular canal: literature review and case report. Dento maxillo facial radiology. 34, 55-58.
- 4.Sonneveld K A, Mai P T, Hogge M, Choi E Y, Portnof J E.Bifid Mandibular Canal: A Case Review and Retrospective Review of CBCTs.
- 5.Orhan K, Aksoy S, Bilecenoglu B, Sakul B, Paksoy C. (2011) Evaluation of bifid mandibular canals with cone-beam computed tomography in a Turkish adult population: a retrospective study. Surg Radiol Anat. 33, 501-507.
- 6.Carter R, Keen E. (1971) The intramandibular course of the inferior alveolar nerve. , J Anat 108, 433-440.
- 7.Moiseiwitsch J. (1998) Position of the mental foramen in a North American, white population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 85, 457-460.
- 8.Wadu S, Penhall B, Townsend G. (1997) Morphological variability of the human inferior alveolar nerve. Clin Anat. 10, 82-87.
- 9.Rouas P, Nancy J, Bar D. (2007) Identification of double mandibular canals: literature review and three case reports with CT scans and cone beam CT. Dento maxillo facial radiology. 36, 34-38.
- 10.Auluck A, Pai K, Shetty C. (2005) Pseudo bifid mandibular canal. Dento maxillo facial radiology. 34, 387-388.
- 11.Mizbah K, Gerlach N, Maal T J, Bergé S, Meijer G. (2012) The clinical relevance of bifid and trifid mandibular canals. Oral Maxillofac Surg. 16, 147-151.
- 12.Fukami K, Shiozaki K F, Mishima A, Kuribayashi A, Hamada Y et al. (2012) Bifid mandibular canal: confirmation of limited cone beam CT findings by gross anatomical and histological investigations. Dentomaxillofac Radiol. 41, 460-465.
- 13.Villaça-Carvalho M, Manhães L, M de, Lopes S. (2016) Prevalence of bifid mandibular canals by cone beam computed tomography. Oral Maxillofac Surg. 20, 289-294.
- 14.Klinge B, Petersson A, Maly P. (1989) Location of the mandibular canal: comparison of macroscopic findings, conventional radiography, and computed tomography. Int J Oral Maxillofac Implants. 4, 327-332.
- 15.Sanchis J, Penarrocha M, Soler F. (2003) Bifid mandibular canal. J Oral Maxillofac Surg. 61, 422-424.
- 16.Kasabah S, Modellel Y. (2014) Classification of bifid mandibular canals in the Syrian population using panoramic radiographs. East Mediterr Health. 19, 178-183.
- 17.Kuczynski A, Kucharski W, Franco A, Westphalen F, AA de L et al. (2014) Prevalence of bifid mandibular canals in panoramic radiographs: a maxillofacial surgical scope. Surg Radiol Anat. 36, 847-850.
- 18.Kalantar Motamedi MH, Navi F, Sarabi N. (2015) Bifid mandibular canals: prevalence and implications. J Oral Maxillofac Surg. 73, 387-390.
- 19.Rashsuren O, Choi J, Han W, Kim E. (2014) Assessment of bifid and trifid mandibular canals using cone-beam computed tomography. Imaging Sci Dent. 44, 229-236.
- 20.Kang J H, Lee K S, Oh M G. (2014) The incidence and configuration of the bifid mandibular canal in Koreans by using cone-beam computed tomography. Imaging Sci Dent. 44, 53-60.
- 21.Naitoh M, Hiraiwa Y, Aimiya H, Ariji E. (2009) Observation of bifid mandibular canal using cone-beam computerized tomography. Int J Oral Maxillofac Implants. 24, 155-159.
- 22.Zhang Y Q, Zhao Y N, Liu D G, Meng Y, Ma X C. (2018) Bifid variations of the mandibular canal: cone beam computed tomography evaluation of 1000 Northern Chinese patients. Oral surgery, oral medicine, oral pathology and oral radiology. 126, 271-278.
- 23.Nortjé C, Farman A, Grotepass F. (1977) Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg. 15, 55-63.
- 24.Langlais R, Broadus R, Glass B. (1985) Bifid mandibular canals in panoramic radiographs. , J Am Dent Assoc 110, 923-926.
- 25.Kikuta S, Iwanaga J, Nakamura K, Hino K, Nakamura M et al. (2018) The retromolar canals and foramina: radiographic observation and application to oral surgery. Surg Radiol Anat. 40, 647-652.
- 26.Lew K, Townsen G. (2006) Failure to obtain adequate anaesthesia associated with a bifid mandibular canal: a case report. Aust Dent J. 51, 86-90.
- 27.Haghighat A, Jafari Z F, Hasheminia D, Samandari M, Safarian V et al. (2015) Comparison of success rate and onset time of two different anesthesia techniques. Med Oral Patol Oral Cir Bucal. 20, 459-463.
- 28.Bilecenoglu B, Tuncer N. (2006) Clinical and anatomical study of retromolar foramen and canal. J Oral Maxillofac Surg. 64, 1493-1497.
- 29.Singh S. (1981) Aberrant buccal nerve encountered at third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 52-142.
- 30.Yamada T, Ishihama K, Yasuda K. (2011) Inferior alveolar nerve canal and branches detected with dental cone beam computed tomography in lower third molar region. , J Oral Maxillofac Surg 69, 1278-1282.
- 31.C de O-S, Souza P, Berti-Couto de A, S. (2012) Assessment of variations of the mandibular canal through cone beam computed tomography. , Clin Oral Investig 16, 387-393.
- 32.Correr G, Iwanko D, Leonardi D, Ulbrich L, Araujo M et al. (2013) Classification of bifid mandibular canals using cone beam computed tomography. Braz Oral Res. 27, 510-516.