Morphological Study of the Posterior Tibial Nerve in Tarsal Tunnel of the Human Foot
Abstract
The passage of the posterior tibial nerve in the tarsal tunnel has a great clinical significance, thus detailed anatomical knowledge is mandatory for safe clinical intervention. This study was to identify the morphological appearance of the tibial nerve and its bifurcation. Sixty lower limbs of formalin embalmed cadavers were randomly selected. Data were collected through the application of standard dissection method of the tarsal tunnel of lower limbs (30 rights and 30 left) of formalin embalmed cadavers. The posterior tibial nerve and its branches were exposed from the distal end of the leg toward plantar surface beyond its bifurcation by resecting the skin and flexor retinaculum. The study triggered several findings: The posterior tibial nerve is flattened shaped in 21 specimens 70% and has a rounded shape in 9 specimens 30%in the right foot. In the left foot it is flattened in 17 specimens 56.7% and rounded shape in 13 specimens 43.3%. Posterior tibial nerve bifurcates into medial and lateral planter nerves inside tarsal tunnel in 20 specimens 66.7% in the right foot and in 21 specimens 70% in the left foot. This study concludes that posterior tibial nerve commonly has flattened shape and divided into medial and lateral planter nerves inside tarsal tunnel.
Author Contributions
Academic Editor: Yi Zhang, Beijing University of Chinese Medicine, China.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Khalid Musa Fadlelmula Awadelseid
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Tarsal tunnel is the term used to describe the area at medial side of the ankle joint where the tendons of the flexor muscles pass from the leg to the sole of the foot with the tibial nerve and posterior tibial vessels between them, fixed in their position by flexor retinaculum 1.
The roof of the tarsal tunnel is formed by the flexor retinaculum and the floor is formed by the medial surface of the talus, the sustentaculum tali the superficial and deep aponeurosis of the leg 1.
The structures pass through the tunnel arranged from medial side are tendon of the tibialis posterior, tendons of the flexor digitorum longus, posterior tibial artery, tibial veins on each side of the artery, tibial nerve, and tendon of the flexor hallucis longus 2.
Tibial nerve is the larger terminal branch of sciatic nerve and is derived from the ventral rami of fourth lumbar (L4), fifth lumbar (L5), first sacral (S1), second sacral (S2), third sacral (S3) roots. It arises at the apex of popliteal fossa and descends in the popliteal fossa to the distal border of popliteus. In the leg, tibial nerve is medial to posterior tibial vessels initially, and then it crosses behind them and descends lateral to them until it bifurcates. Tibial nerve ends by dividing into medial and lateral plantar nerves beneath the flexor retinaculum 1, 2.
Anatomy of the posterior tibial nerve (PTN) in the tarsal tunnel has important clinical significance; entrapment of the PTN causes tarsal tunnel syndrome which may relate to position and shape of the nerve. Tarsal tunnel used as portal for arthroscopy 3.Nails to fix lower tibia pass through this area 4. 5, 6.
Aim of this study was to identify the morphological appearance of the PTN, and to locate the position of its division. Thus, detailed anatomical knowledge is important so as to identify safe zone for surgical intervention in this area.
Material and Methods
Materials for this study were collected from randomly selected 30 formalin embalmed human cadavers from anatomy departments of Jazan and Alexandria Universities (60 specimens), 8 female and 22 male, age between 35-73 years, causes of death unknown.
Data was collected by dissection of 30 right foot and 30 left foot. A reference line of 1 cm width, medio malleolar calcaneal axis‟ (MMCA) made with transparent plastic sheet was placed from the tip of the medial malleolus of tibia to the medial tubercle of calcaneus this was used as grid to classify the bifurcation level of posterior tibial nerve into Type I, II and III. Type I, II, III represented the bifurcations proximal to, deep to and distal to axis respectively (Figure 1).
Skin was incised at distal end of the leg to the planter surface of the foot and reflected. Subcutaneous tissue was removed. Deep fascia along with the flexor retinaculum was cut, and the PTN was exposed structures were separated from the nerve. The tibial nerve and posterior tibial artery along with venae comitantes were exposed from the distal end of leg towards plantar surface beyond its bifurcation by resecting the abductor hallucis muscle (Figure 1).
Figure 1.Medio Malleolar Calcaneal axis‟ (MMC axis) made by transparent plastic sheet in the left foot, (MM): Medial Malleolus, (C): Medial tubercle of calcaneus.
Shape of PTN was noted and its division was identified according to medio malleolar calcaneal axis (MMCA).
A check list was designed and the data were collected. Data were analyzed using IBM SPSS software package version 20.0.Many tests were used to describe the qualitative and quantities data. Marginal Homogeneity Test used to compare between right and left side. Kolmogorov-Smirnov test, Shapiro-Wilk test and D'Agstino test were used for normality distribution. Parametric tests applied for normal data distribution. Non-parametric tests used in abnormally distributed data. For normally distributed data, paired t-test is used to analyze two paired data, for abnormally distributed data, Wilcoxon signed ranks test is used to analyze two paired data 7, 8.
Results
The TN is flattened just before its bifurcation in 21 specimens (70%) and has a rounded shape in 9 specimens (30%) in the right foot. In the left foot it is flattened in 17 specimens 56.7% and rounded shape in 13 specimens 43.3% (Table 1; Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7, Figure 8).
Table 1. Shape of the Posterior Tibial Nerve.| Foot | MH c 2 | P | ||||
| Right (n = 30) | Left (n = 30) | |||||
| NO | % | NO | % | 1.155 | 0.248 | |
| Flattened | 21 | 70 | 17 | 56.7 | ||
| Rounded | 9 | 30 | 13 | 43.3 | ||
Figure 2.Showing shape of the PTN
Figure 3.A, B, C, and D showing the flattened shape of the PTN in tarsal tunnel PTN= Posterior Tibial nerve
Figure 4.(A), (B) & (C) showing rounded shape of the PTN.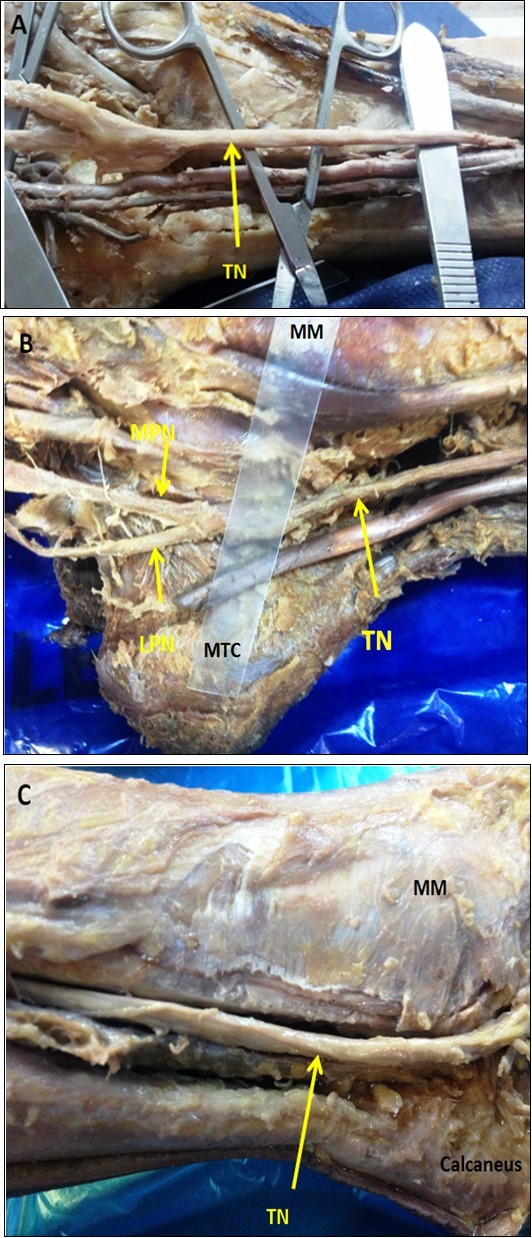
Figure 5.Sowing the types of PTN. 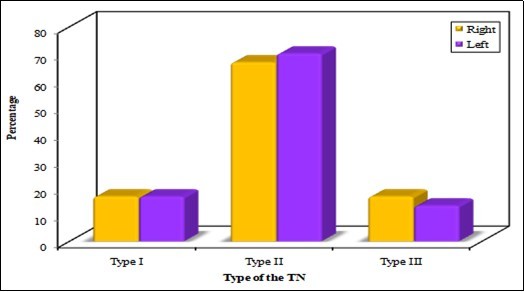
Figure 6.Showing PTN divided into Medial and lateral planter nerves outside tarsal tunnel (type I TN).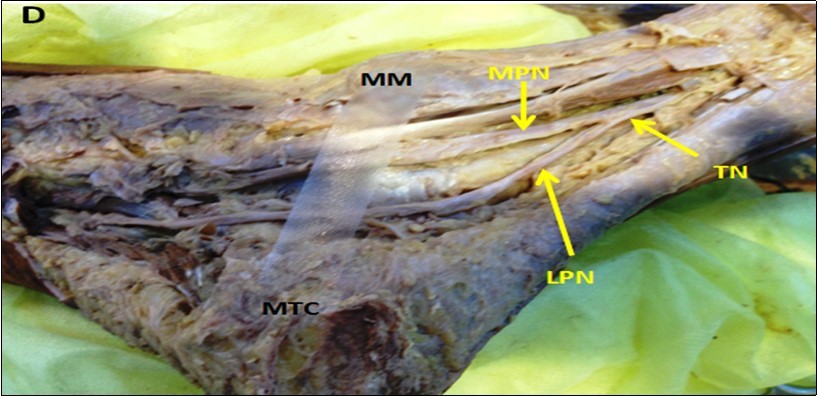
Figure 7.showing PTN bifurcates inside the tarsal tunnel (Type II PTN)
Figure 8.Showing PTN bifurcates distal to the MMCA (Type III TN)
According to MMCA, the PTN bifurcates proximal to this axis which represents the flexor retinaculum (means that the PTN bifurcates outside tarsal tunnel (TT) as type I in 5 specimens (16.7%) behind to the axis (inside TT) type II in 20 specimens (66.7%), and distal to the axis (outside TT) type III in 5 specimens (16.7%) in the right foot. In the left foot the PTN divides in the TT as type II in 21specemins 70%, type I in 5 specimens (16.7%), and type III in 13.3%.
Discussion
Anatomy represents the inlet for understanding clinical medicine and surgery 9.The tarsal tunnel has great clinical significance; it is the portal of the foot many structures pass from the leg to the foot. As well it is used as medial portal for arthroscopy, thus studding anatomy of the PTN in this area may give important information which can help in explanation of many clinical conditions such as tarsal tunnel syndrome and may help clinicians to identify safe zone on medial side of the ankle joint during surgical procedures.
The TN in the present study showed a flattened shape just before its bifurcation in 21 specimens 70% and has a rounded shape in 9 specimens 30% in the right foot. In the left foot it is flattened in 17 specimens 56.7% and rounded shape in 13 specimens 43.3% these results nearly in agreement with Joshi et al described a flattened shape of the TN in 57.14% in the right foot and Lt 58.92% in the left foot 10. From the result of this study we can say that the flattened shape is most common presentation than rounded shape, and we need further clinical investigations among patients who suffer from tarsal tunnel syndrome due to compression of the PTN which defined firstly by Lam and Keck 11.To detect which shape is liable to entrapment in the tarsal tunnel. There is no enough literature to decide that the flattened shape is normal or due to mechanic effect at the ankle joint.
In the present study, a reference line of 1 cm width, mediomalleolar calcaneal axis‟ (MMCA) made with transparent plastic sheet was placed from the tip of the medial malleolus of tibia to the medial tubercle of calcaneus. This was used as grid to classify the bifurcation level of PTN into Type I, II and III which represented the bifurcation proximal to, deep to and distal to this axis respectively. The present study was done to identify the level of bifurcation of PTN based on MMCA.
In the present study, the PTN was present as type I in (16.7%) type II in (66.7%) and type III in (16.7%) in the right foot, in the left foot (16.7%), (70%), and (13.3%) respectively. From these results type II PTN is the common presentation. This means that PTN bifurcates into MPN and LPN commonly within the tarsal tunnel. In agreement with Dellon et al in 90% of specimens 12, Havel et al in 93% of specimens 13, Davis et al (68.7%) 14 and Moraes et al 72.4% 15 and Ndiaye et al in (90%) of specimens 16.
Proximal bifurcation of the TN (type I) outside the tarsal tunnel occurred in (16.7%) in the present study. This result is contradicted by the observations of Joshi et al 10, Fernandes et al 17,Louisia et al18 and Bilge et al 19; they reported that proximal bifurcation of the TN occurred in (100%), (74.4%), (85.2%), (84%) respectively. The discrepancy with these studies can be explained by the differences in width of the MMCA; some authors used one line or two lines to represent the axis. In the present study, a transparent plastic sheet of 1cm width is measured precisely to be used as grid for classification of the bifurcations of the PTN.
Distal bifurcation of the TN (type III) in the present study is 16.7% and 13.3% in right and left foot respectively this result coincide with Horwitz et al 16.2% 20, Govsa et al 21.6% , 21,Dellon in 16.13% 12,Joshi et in 8.9%, 10,and Bilge in 4%, 17. Hegazy and Hailal found the safest area for surgical approach to ankle joint is the area in-between the two tibialis muscles below the medial malleolus; and named this triangle the foot anatomical box 22.We might agree them as the neurovascular bundle as well as bifurcation of PTN in the current study are situated on the inner aspect of such area.
Conclusions
From the results of this study, it could be concluded that flattened shape of the PTN is common presentation and bifurcation into MPN and LPN commonly occurred in the tarsal tunnel.
Recommendations
Clinicians should be aware of the variable location of the PTN bifurcation during any surgical intervention in the tarsal tunnel. Further investigations are needed concerning shape of the PTN to identify its association with the entrapment of the nerve in the tarsal tunnel.
Abbreviations
PTN: Posterior tibial nerve
MPN: Medial planter nerve
LPN: Lateral planter nerve
MMCA: Mediomalleolar calcaneal axis.
Acknowledgment
Author would like to express his gratitude to the heads of anatomy departments in Alexandria and Jazan Universities for their permission to dissect the specimens, and to my colleagues for their valuable advices.
References
- 1.Standring S. (2008) Gray's Anatomy. The anatomical basis of clinical practice. 40th ed London: Churchill Livingstone. 1425-30.
- 2.Snell R. (2012) Clinical anatomy by regions. 9th ed. , Baltimore, Md: Lippincott Williams 479-481.
- 3.Lijoi F, Lughi M, Baccarani G. (2003) Posterior arthroscopic approach to the ankle: An anatomic study. Arthroscopy. 19, 62-67.
- 4.Hromádka R, Barták V, Popelka S, Pokorný D, Jahoda D et al. (2010) Ankle block implemented through two skin punctures. Foot Ankle Int. 31(7), 619-23.
- 5.Sitler D F, Amendola A, Bailey C S, Thain L M, Spouge A. (2002) Posterior ankle arthroscopy: An anatomic study. , J Bone Joint Surg Am 84, 763-9.
- 7.Kirkpatrick L A, Feeney B C. (2013) A simple guide to IBM SPSS statistics for version 20.0. Student ed. , Belmont, CA:Wadsworth, Cengage Learning
- 8.Kotz S, Balakrishnan N, Read C B, Vidakovic B. (2006) Encyclopedia of statistical sciences. 2nd ed. , Hoboken, NJ:Wiley-Interscience;
- 9.Hegazy A A. (2019) Human Anatomy: An Inlet of Medicine and Surgery. , International Journal of Human Anatomy 1(4), 1-1.
- 10.Joshi S S, Joshi S D, Athavale S A. (2006) Anatomy of tarsal tunnel and its applied significance. J AnatSoc India. 55(1), 52-6.
- 12.Dellon A L, Mackinnon S E. (1984) Tibial nerve branching in the tarsal tunnel. , Arch Neurol 41(6), 645-6.
- 13.Havel P E, Ebraheim N A, Clark S E, Jackson W T, Didio L. (1988) Tibial nerve branching in the tarsal tunnel. Foot Ankle. 9(3), 117-9.
- 14.Davis T J, Schon L C. (1995) Branches of the tibial nerve: anatomic variations. Foot Ankle Int. 16(1), 21-7.
- 15.Moraes D C, Carvalho A E, Fialho H S, Galbiatti J A, Carvalho D E. (2007) Nervotibial: variaçõesanatômicas do ramocalcâneo medial. Rev ABTPé. 1(2), 31-40.
- 16.Ndiaye A, Dia A, Konate I, Diop M, Sow M L. (2003) Topographic anatomy of the tibial nerve in the medial malleolus: application to the effect of nerve block anesthesia. Morphologie. 87(277), 25-7.
- 17.RMP Fernandes, Mozella A, Dias M, Carvalho R, Andrade F et al. (2006) Estudoanatômico do nervotibial no túnel do tarso. Rev Bras de Ortop. 41(7), 272-7.
- 18.Louisia S, Masquelet A C. (1999) The medial and inferior calcaneal nerves: an anatomic study. SurgRadiolAnat. 21(3), 169-73.
- 19.Bilge O, Ozer M A, Govsa F. (2003) Neurovascular branching in the tarsal tunnel. Neuroanatomy. 2, 39-41.
- 20.Horwitz M T. (1938) Normal anatomy and variations of the peripheral nerve of the leg and foot: Application in operations for vascular diseases: Study of one hundred specimens. , Arch Surg 36(4), 626-36.
Cited by (2)
This article has been cited by 2 scholarly works according to:
Citing Articles:
Anatomy & Cell Biology (2023) OpenAlex
Anatomy & Cell Biology (2023) Crossref